From Neuroscientifically Challenged, this is an excellent explainer on the state of research into depression, including the rise and fall of the serotonin theory and the rise and struggle of the neurogenesis model. Fortunately, there is science, and the scientific method.
Serotonin, depression, neurogenesis, and the beauty of science
If you asked any self-respecting neuroscientist 25 years ago what causes depression, she would likely have only briefly considered the question before responding that depression is caused by a monoamine deficiency. Specifically, she might have added, in many cases it seems to be caused by low levels of serotonin in the brain. The monoamine hypothesis that she would have been referring to was first formulated in the late 1960s, and at that time was centered primarily around norepinephrine. But in the decades following the birth of the monoamine hypothesis, its focus shifted to serotonin, in part due to the putative success of antidepressant drugs that targeted the serotonin transporter (e.g. selective serotonin reuptake inhibitors, or SSRIs). The monoamine/serotonin hypothesis eventually became generally recognized as viable by the scientific community. Interestingly, it also became widely accepted by the public, who were regularly exposed to television commercials for antidepressant drugs like Prozac, Lexapro, and Celexa--drugs whose commercials specifically mentioned a serotonin imbalance as playing a role in depression.Over the years, however, the scientific method quietly and efficiently went to work. Evidence gradually accumulated that indicated that the serotonin hypothesis does a very inadequate job of explaining depression. For example, although SSRIs increase serotonin levels within hours after drug administration, if their administration leads to beneficial effects--a big if--it usually takes 2-4 weeks of daily administration for those effects to appear. One would assume that if serotonin levels were causally linked to depression, then soon after serotonin levels increased, mood would begin to improve. Also, reducing levels of serotonin in the brain does not cause depression. The list of studies that don't fully support the serotonin hypothesis of depression is actually quite lengthy, and most of the scientific community now agrees that the hypothesis is insufficient as a standalone explanation of depression.
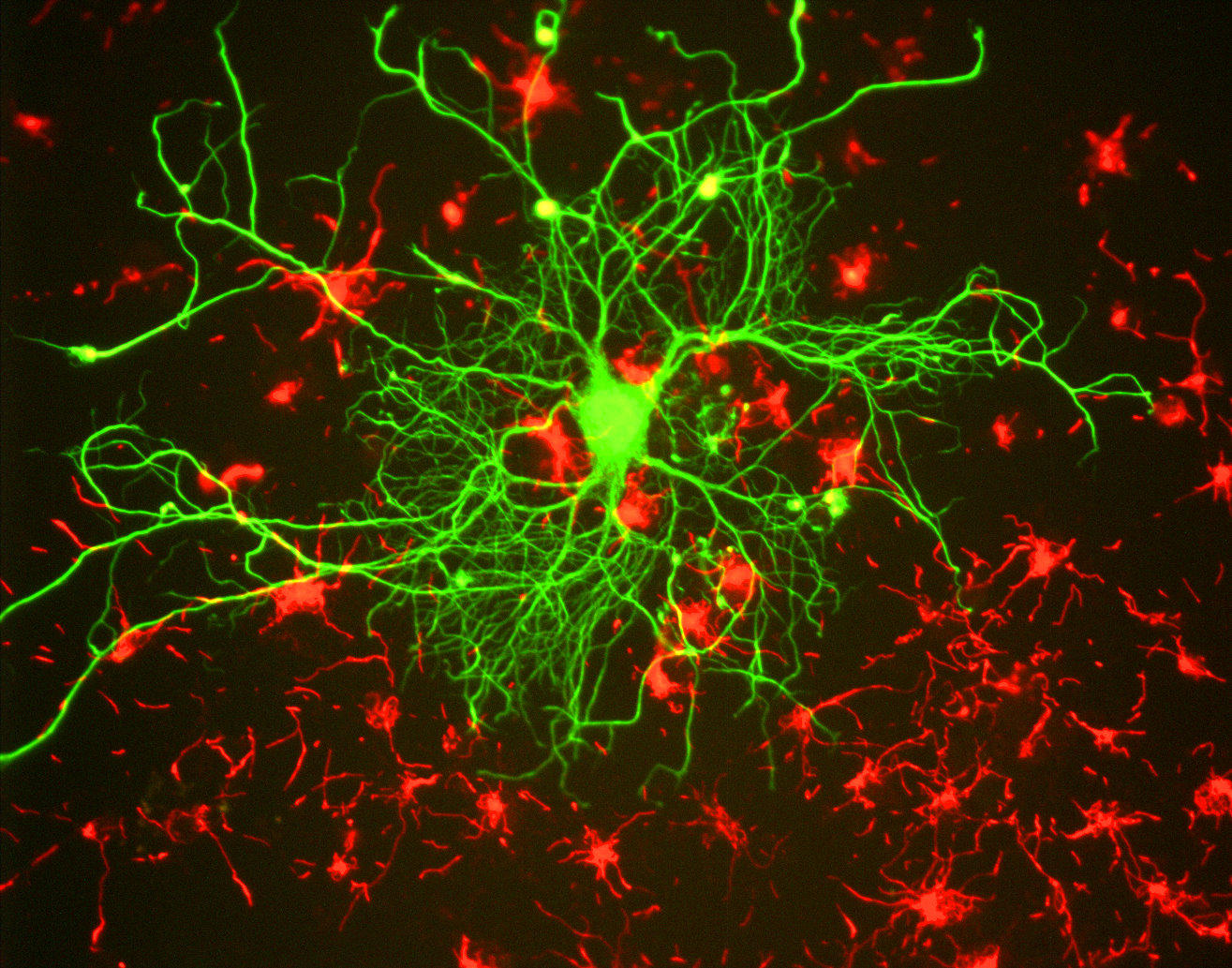
In the 1990s another hypothesis, known as the neurogenic hypothesis, was proposed with the hopes of filling in some of the holes in the etiology of depression that the monoamine hypothesis seemed to be unable to fill. The neurogenic hypothesis suggests that depression is at least partially caused by an impairment of the brain's ability to produce new neurons, a process known as neurogenesis. Specifically, researchers have focused on neurogenesis in the hippocampus, one of the only areas in the brain where neurogenesis has been observed in adulthood (the other being the subventricular zone).
The neurogenic hypothesis was formulated based on several observations. First, depressed patients seem to have smaller hippocampi than the general population, and their hippocampi also appear to be smaller during periods of depression than during periods of remission. Second, glucocorticoids like cortisol are elevated in depression, and glucocorticoids appear to inhibit neurogenesis in the hippocampus in rodents and non-human primates. Finally, there is evidence that the chronic administration of antidepressants increases neurogenesis in the hippocampus in rodents.
The neurogenic hypothesis thus suggests that depression is associated with a reduction in the birth of new neurons in the hippocampus, an area of the brain important to stress regulation, cognition, and mood. According to this hypothesis, when someone takes antidepressants, the drugs do raise levels of monoamines like serotonin, but they also enact long-term processes that increase neurogenesis in the hippocampus. This neurogenesis is hypothesized to be a crucial part of the reason antidepressants work, and the fact that it takes some time for hippocampal neurogenesis to return to normal may help to explain why antidepressants take several weeks to have an effect.
This may all sound logical, but the neurogenic hypothesis has its own share of problems. For example, while stress-related impairment of neurogenesis has been observed in rodents, we don't have definitive evidence it occurs in humans. Human studies thus far have relied on comparing the size of the hippocampi in depressed and non-depressed patients. While smaller hippocampi have been observed in depressed individuals, it is not clear that this is due to reduced neurogenesis rather than some other type of structural changes that might have occurred during depression.
Similarly, while the administration of antidepressants has been associated with increased neurogenesis in rodent models of stress, we don't have clear evidence of this in humans. In humans we again have to rely on looking at things like hippocampal size. Because there could be a number of explanations for changes in the size of the hippocampi, we can't assume neurogenesis is the sole factor involved--or that it is involved at all. Additionally, some studies in rodents have found that antidepressants lead to a reduction in anxiety or depressive symptoms in the absence of increased hippocampal neurogenesis.
Another problem is that when neurogenesis is experimentally decreased in rodents, the animals don't usually display depressive symptoms. Experiments of this type haven't been performed with humans or non-human primates, so we don't know if a reduction in neurogenesis in any species is actually sufficient to cause depression. And no studies have found that increasing neurogenesis alone is enough to alleviate depressive-like symptoms.
Of course none of this means the neurogenic hypothesis is incorrect, but it does suggest there is a long way to go before we can feel confident about incorporating it fully into our understanding of depression. In the reluctance of the scientific community to embrace this hypothesis is where I see the beauty of science. Although it took decades of testing and revising before the monoamine hypothesis became a widely accepted explanation for depression, one could argue (based on its now recognized shortcomings) that we accepted it too readily.
However, it seems that many in the scientific community have learned from that mistake. Although there is no shortage of publications whose authors may be too willing to anoint the neurogenic hypothesis as a new unifying theory of depression, overall the tone when speaking of the neurogenic hypothesis seems to be cautious and/or critical. There is also a great deal of discussion now in the literature about the complexity of mood disorders like depression, and how it is unlikely to be able to explain their manifestation in a diverse population of individuals with just one mechanism, whether it be impaired neurogenesis or a serotonin deficiency.
Thus, the neurogenic hypothesis will require much more testing before we can consider it an important piece in the puzzle of depression. Even if further testing supports it, however, it will likely be considered just that--a piece in the puzzle, instead of an overarching explanation of the disorder. And that circumspect approach to explaining depression represents an important advancement in the way we look at psychiatric disorders.
See also: http://www.neuroscientificallychallenged.com/blog/2008/04/serotonin-hypothesis-and-neurogenesis
Miller, B., & Hen, R. (2015). The current state of the neurogenic theory of depression and anxiety Current Opinion in Neurobiology, 30, 51-58 DOI: 10.1016/j.conb.2014.08.012
No comments:
Post a Comment